Automating Claims and Payments through Oracle Health EHR Integration with Insurance Providers
Application Integration
Overview
A leading healthcare provider in Dubai partnered with Tellestia to modernize its claims and payments operations by integrating its Oracle Health EHR Revenue Cycle Management (RCM) module with multiple UAE health insurance providers. The initiative focused on revenue cycle management automation, improved healthcare interoperability, and secure data exchange using an API-led integration powered by the WSO2 integration platform.
The project connected the hospital’s RCM with major insurers including Next Care, Saada Insurance, NGI, NAS, FMC, and MSH International - enabling fully automated claim submissions, pre-authorizations, and payment reconciliation while maintaining compliance and security across the healthcare interoperability platform.
The Challenge
Key challenges included:

Business Challenges
- Manual claims submission created administrative overhead, delays, and increased cost of operations.
- Frequent denials due to human errors and payer-specific rule inconsistencies.
- Limited real-time visibility into claim status affected financial forecasting.
- Manual pre-authorizations slowed critical treatments and negatively impacted patient experience.
- Each payer had unique coding and submission requirements, making compliance complex.
Technical Challenges
- Different insurers relied on APIs, portals, or legacy file-based workflows.
- Mapping clinical data from the medical EHR software to payer-compliant EDI formats (e.g., X12).
- Ensuring secure health data exchange and compliance with healthcare data standards.
- Managing errors and retries across multiple payer systems without interrupting hospital operations.
The Objective
The key objective of this initiative included:

- Implement end-to-end healthcare claims automation from submission to status tracking and payments.
- Standardize and automate pre-authorization processes to accelerate patient care.
- Reduce denials through data validation, transformation, and payer-specific rule enforcement.
- Enable real-time visibility of claim statuses within Oracle Health EHR.
- Strengthen compliance and security for sensitive patient data exchange using modern healthcare API management practices.
The Solution
Tellestia designed a centralized integration hub leveraging the WSO2 integration platform to serve as a secure middleware layer between Oracle Health EHR and multiple insurance providers. This architecture delivered scalable, API-led connectivity while supporting both modern and legacy integration methods.
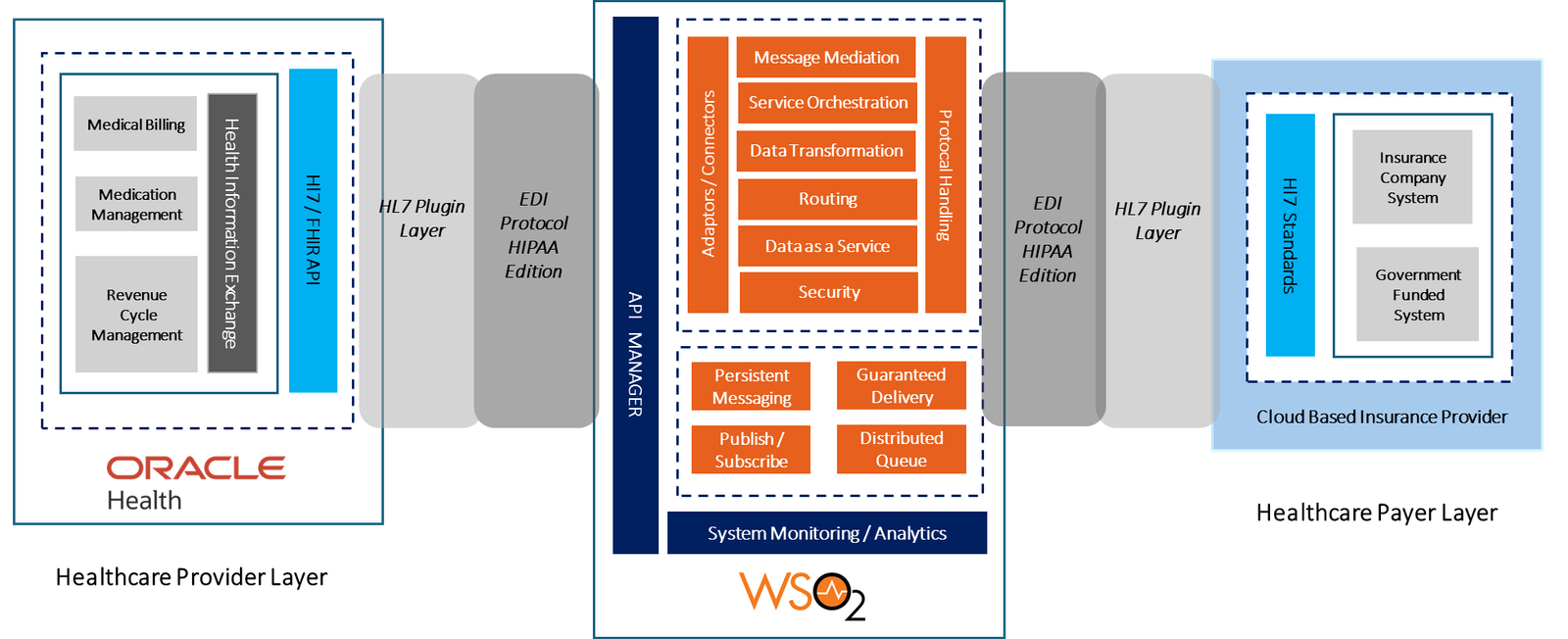
Key Solution Components include:
- Oracle Health EHR RCM: Source of patient, encounter, diagnosis (ICD-10), and CPT procedure data, operating as the core healthcare EHR system.
- WSO2 Integration Layer: Middleware for orchestrating workflows, handling EDI transformations, and managing secure API and sFTP connections.
- EDI Engine: Automated conversion to payer-compliant formats such as X12 837 (claims) and X12 278 (pre-authorization).
- Insurance Provider Connectivity: Direct API integration for modern insurers and secure file-transfer workflows for legacy platforms, enabling seamless health insurance API integration.
Core Workflows Implemented
The integration solution delivered immediate, impactful results:
- Automated Claims Submission
- Initiated from finalized encounters in Oracle Health EHR.
- Validated and transformed into payer-specific EDI formats.
- Securely transmitted via API or sFTP.
- Real-time acknowledgments updated directly in the RCM module.
- Pre-Authorization Requests
- Automated transformation of physician orders into payer-specific authorization formats.
- Real-time responses (approved, denied, pending) updated within the EHR.
- Claims Status Updates
- Bidirectional integration to instantly update billing teams on claim progress and denials.
- Eliminated the need to log into multiple insurer portals.
- Security & Compliance
- OAuth 2.0 authentication for API/interoperability workflows.
- Full end-to-end encryption supporting highly secure health data exchange.Detailed audit logging aligned with regional and international healthcare compliance requirements.
The Impact

- Faster Revenue Cycle: Automated submissions and live data exchange accelerated claim processing and payments.
- Lower Denial Rates: Rule-driven validation and Revenue Cycle Management automation minimized rejections.
- Improved Patient Experience: Faster pre-authorizations led to timely clinical decisions.
- Operational Efficiency: Reduced administrative burden enabled staff to focus on patient care rather than manual systems.
- Financial Transparency: Real-time visibility across the claims lifecycle improved cash flow predictability and planning.

Let’s Get Started on Your Transformation Journey.
You Might Also Like

East African Bank Integrates REGIDESO Utility Payments with WSO2
An East African bank streamlines REGIDESO utility payments through real-time WSO2 integration with Tellestia.
Read Story
Fueling Government Innovation with MuleSoft-Powered Digital Integration
A leading public sector entity recognized the need to address functional silos, data duplication, and interoperability challenges to improve operational...
Read Story
Transforming Payment Infrastructure for a Middle Eastern Bank with Finastra Fusion P2G
A Middle Eastern bank achieved real-time, compliant payments with Finastra P2G and Tellestia’s scalable transformation platform.
Read Story